In the field of psychology, the term “schizophrenia” is now widely used because research in this area is making a greater effort to understand its existence. There are various other disorders that fall under the spectrum of schizophrenia. Based on the symptoms that patients typically exhibit, these are differentiated and characterised in different ways. It is critical to document the symptoms and seek assistance as soon as possible. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) states that if a patient exhibits any of the symptoms listed below, they are diagnosed with schizophrenia.
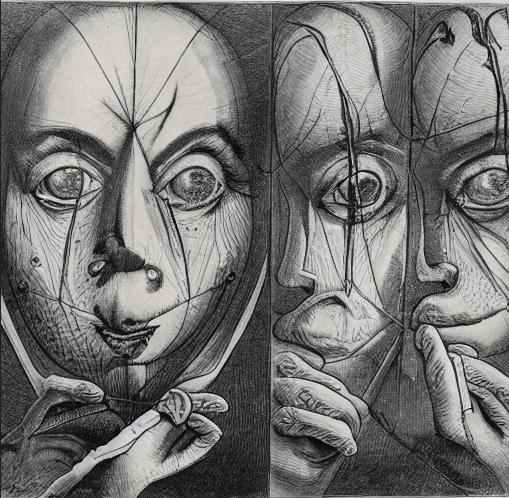
Table of Contents
- Delusions: these are people’s unfounded beliefs that have no bearing on the real world. like thinking that someone might be attempting to murder them.
- Hallucinations: People may experience hallucinations, in which they perceive objects that are not actually there. Like hearing or seeing a person.
- Catatonic behaviour: people who are unable to respond to their surroundings and stay fixed. Like engaging in repetitive behaviour.
- Disorganized thoughts: the individual has difficulty with thought building and processing; their words may come out jumbled and difficult to understand. The above are positive symptoms, as they are visible and can be noted during the session by the interviewer. Unlike the negative symptoms, they do not interfere with the diurnal activity of the individuals.
- Negative symptoms: include loss of normal functioning, loss of speech, and even a lack of facial expression.
The DSM includes this spectrum of schizophrenic disorders.
- Schizotypal personality disorder
- Schizoaffective disorder
- Delusional disorder
- Medicine/substance-induced psychotic disorder
- Schizophrenia
- Brief psychotic disorder
- Psychotic disorder occurring due to other medical condition
- Catatonia associated with other mental disorder
- Unspecified schizophrenia spectrum and other psychotic disorders
1. Schizotypal personality disorder
A person with this disorder usually exhibits unusual behaviour. The people struggle greatly to establish and preserve intimate, personal relationships. They tend to rely on their strong, odd beliefs and superstitions. Delusions and hallucinations happen occasionally, but not as frequently as in schizophrenia. People who suffer from schizotypal personality disorder find it difficult to interact amicably with anyone outside of their close family. They are anxious; they usually have paranoid thoughts and consistent doubt about the other person’s loyalty.
2. Schizoaffective disorder
Multiple symptoms found in the DSM-schizophrenia spectrum, such as delusions and hallucinations, are indicative of this disorder. Apart from the other symptoms, they also display odd behaviour, difficulty speaking, and difficulty meeting their basic needs.
3. Delusional disorders
Delusional disorders are mainly defined for people who have frequent episodes of delusions, like believing things that do not have any connection to or relate to reality whatsoever. With the onset of the symptoms, the individual finds it difficult to distinguish between reality and false superstitions. Their functionality, however, remains unaffected.
4. Medicine- /substance-induced psychotic disorder
The main cause of this illness is the start or stop of specific medications, which can result in symptoms like agitation, hallucinations, aggressive thoughts, and suicidal thoughts. Methamphetamine, cannabis, and opioids are just a few of the substances that can cause this illness. The use of cannabis is seen to have an effect on the psychosis of the individual. The treatment is not yet specified; however, the patient is carefully monitored, and a dose of an antipsychotic drug is given.
5. Schizophrenia
The difference between schizophrenia and the other disorders mentioned is that it is a lifelong condition. The symptoms tend to be vivid since the late teenage or early 20s, which include:
- Agitation
- Lack of sleep
- Withdrawal from social interaction
- Anxiety
- Difficulty in concentrating
- Strange ideas
The causes of schizophrenia are still unknown, but researchers believe that environmental and genetic conditions vastly influence the disorder. Antipsychotic drugs play a vital role in reducing the symptoms of the disorder. The cure is not affixed, but psychotherapy has helped the patients deal with the situations appropriately. Cognitive therapy (CBT) is a type of psychotherapy in which the therapist helps the patient look at situations closely. Over the multiple number of sessions, the patient is helped to gain a different perspective. It is more about adopting positive thoughts and unlearning negative, bothersome, and bizarre thoughts.
6. Catatonia associated with other psychotic disorders
A psychomotor disorder, catatonia, hinders a person’s ability to move. Its pathobiology is still unknown, but it is regarded as a serious mood disorder. However, it is suspected to be GAMA (gamma-aminobutyric acid) and glutamate.
Neuroimaging pointed out:
- I. Reduced resting state activity
- II. Reduced task activation
Individuals suffering from hyperkinetic catatonia may engage in self-harming behaviours as well as restless, agitated behaviour. However, the most prevalent type of catatonic disorder, known as akinetic catatonia, is characterised by slowed behaviour; the patient frequently nods off and stares into space.
The causes of the disorder are neurodevelopmental disorder, bipolar disorder, psychotic disorder, etc.
The symptoms of catatonia include:
- Inability to move or speak
- Malnourishment and dehydration
- Muscle rigidity(catalepsy)
- Agitation
- Restlessness
- In malignant kind of catatonia, symptoms are:
- Delirium
- Fever
- Rigidity
The treatment includes electroconvulsive therapy (ECT), in which the patient is sedated and given brain shocks that induce seizures in the brain. It is a painless procedure. It is also suggested that catatonic patients should avoid taking neuroleptic drugs.
7. Schizophrenic spectrum and other related psychotic disorders
The primary symptom of this condition is psychosis, which includes hallucinations and delusions. Loss of motivation, social withdrawal, disinterest in daily life, and difficulty displaying emotions are some of the symptoms of this condition. The associated disorders share the same symptoms as those of schizophrenia. The associated conditions are:
- Major depressive disorder
- Bipolar disorder
- Post-traumatic stress disorder
- Autism spectrum disorder
- Substance use disorder
- Dementia

How does living with schizophrenia interfere with daily life?
People who have the aforementioned illnesses deal with numerous challenges on a daily basis. In no way do their circumstances resemble those of people who lead regular lives. They also become disinterested in a number of their activities and chores as a result of their inability to maintain focus. They experience constant waves of anxiety and find it extremely difficult to socialise or take part in any social events. When someone starts to lose interest in their regular activities, it also becomes very difficult for them to take care of themselves. Distressed thoughts and decreased productivity accompany the other negative effects of the disorder.
Which myths exist regarding the disorder?
There are many false beliefs about schizophrenia. It is erroneous to assume that individuals suffering from this illness have two personalities, since dissociative identity disorder is a condition that includes multiple personalities. Second, the general public frequently perceives individuals suffering from schizophrenia as dangerous, which makes them feel intimidated by these patients. Since the patient may or may not exhibit aggression, which is a symptom of schizophrenia, this is utterly absurd. People who suffer from schizophrenia are often referred to as “mad” or “crazy,” which is extremely derogatory. Individuals with this mental illness are unable to control their own behaviour. Rather than isolating individuals with these illnesses, we must identify their symptoms and extend our support to them in order to improve their situation.
Conclusion:
People experiencing this mental illness should be acknowledged and assisted as soon as possible. Getting treatment when needed is equally important to prevent the disorder from getting worse and making it harder for the person to lead a normal life. An approachably methodical form of treatment is provided to individuals with schizophrenia and related disorders in an effort to improve their state of health.
Frequently asked questions:
- What triggers delusional disorder?
A multitude of factors either influence or provoke delusional disorders. Biological factors, such as chemical imbalances in the brain, may also contribute to the disorder in addition to environmental factors. Genetic predispositions or a person’s personal history of the disorder may also have an impact on when the disorder manifests.
- How do you treat delusions in schizophrenia?
Healthcare professionals recommend a course of treatment based on the study after analysing the disorders’ symptoms and their severity. The course of treatment can be continued in multiple ways. The patient is given antipsychotic (also known as a neuroleptic) medication. The other approaches mostly consist of counselling and therapy sessions.
- What type of delusions are most common in schizophrenia?
Delusions of a paranoid nature are the most prevalent kind in patients with schizophrenia. signs and feelings of persecution that accompany these kinds of persistently illogical thoughts.
- Does delusional disorder go away?
There is a chance the illness will go extinct altogether. In order to help the patient recover to a significant degree, treatment is imperative. Research shows that 50% of patients have fully recovered from the disorder, while 20% report essentially no change in symptoms. Numerous internal factors cause the improvement rate to differ from person to person.



